Contributor: Dr Allyson Leacock, Executive Director, LIVE UP: The Caribbean Media Alliance
LIVE UP: The Caribbean Media Alliance brought together key population (KP) advocates (including People Living with HIV, men who have sex with Men, sex workers, and transgender) and media for a workshop to foster alliances for stigma reduction. In its efforts to honour the principles of the Fourth Estate, LIVE UP saw the workshop as an opportunity to continually challenge the status quo and empower as well as enlighten audiences to love, protect and respect all people. Given its 10-year track record of training media how to report responsibly and accurately on the multi-faceted and complex issue of HIV and all the dimensions of sexual and reproductive health and rights, LIVE UP is well placed to educate media further on S&D so that they become unwitting advocates to reduce S&D in our region.
LIVE UP, with funding through a PANCAP small grant from the Local Capacity Initiative funded by USAID, began the process of Creating Alliances for Amplifying Voices to Reduce Stigma and Discrimination and Increasing Access to Non-stigmatizing Services on May 26, 2017 with a Knowledge Café designed to create preliminary connections between media and key population advocates in Barbados. The Café was an opportunity for KP and Media to be apprised of regional initiatives that are working towards achieving the project goals and hearing from regional key players and influencers, namely: Dr. Edward Greene, UNAIDS Advisor, Mr. Dereck Springer, Director of PANCAP, Mr. Ainsley Reid, GIPA Coordinator and Mrs. Gardenia Destang-Richardson, National AIDS Programme Coordinator. They spoke about: a) what is being done at the policy level for KPs and b) how the media can underpin their reporting with this resource information going forward, to ensure their stories are substantiated with solid information.
The third value-added dimension of this Knowledge Café was that it served as an icebreaker for the 2 groups as the first dimension of the workshops providing the Caribbean context to show them the scope of work that needs to be done by both groups to advance the reduction of S&D agenda. We saw this as Part One of the workshops providing valuable regional context. This was filmed and will be given to participants and PANCAP as a part of the Resource Tool that forms part of the project.
The subsequent workshop sessions will be even more hands-on and provide practical exercises and details of advocacy and the multiple media tools available that can be used by advocates, while media will be shown tangible examples of ways to reduce stigma in their reporting, using the approaches they understand.
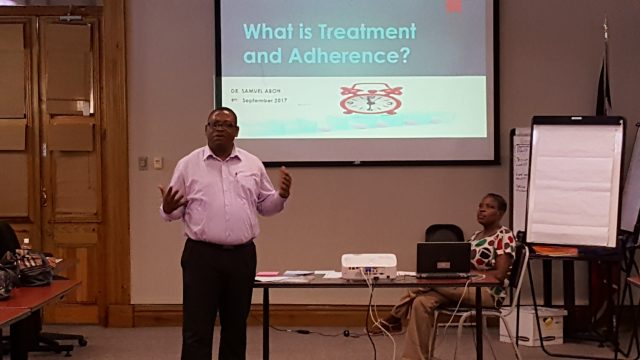
On July 5th & 6th, 2017 LIVE UP hosted a workshop for Key Population advocates and Media practitioners at Almond Bay, Hastings, Barbados. The Key population advocates were invited from several local civil society organisations including BGLAD, EQUALS, HOPEN and JABEZ HOUSE. The media practitioners were from broadcast media partners of LIVE UP. The participant list is attached in Annex B. The workshop was designed and facilitated by Dr. Allyson Leacock Executive Director, LIVE UP: The Caribbean Media Alliance and Ayana Hypolite, Counsellor. The workshop was very well received by both media and KP advocates alike. Their evaluations are appended to this report (via email attachment) at Annex F.
This workshop and the programme that it supports is unique not just in the fact that the mutual benefits of media and KP collaborating were taken into consideration in the planning and execution but also in the fact that LIVE UP has used its grant to not only build its stigma reduction capacity but also to build the capacity of several other local CSOs who are working on stigma reduction programming as well. Giving them the tools as well as the platform with which to amplify their efforts and voices.
AIMS & OBJECTIVES of the workshop:
The broad goals of this workshop were to build the capacity of CSOs in Advocacy and educate Media about S&D, its effects and the ways in which it can be reduced. Together, this would achieve the aims of:
- Increasing understanding of key populations (MSM, Sex Workers, Transgender people and People living with HIV)
- Reducing HIV stigma & discrimination
- Discussing advocacy around HIV and related issues such as sexuality and diversity.
The specific objectives of this workshop were to:
1. To help participants develop an understanding of HIV and key population stigma, its causes and effects on individuals, families and communities
2. To explore different aspects of stigma towards PLHIV, MSM and Sex workers
3. To build alliances among key population CSO and the media for positive change
4. To develop ideas for messaging and campaigns