Tuesday, December 5 2017 (PANCAP Coordinating Unit, CARICOM Secretariat): The Pan Caribbean Partnership against HIV and AIDS (PANCAP), the mechanism that provides a structured and unified approach to the Caribbean’s response to the HIV epidemic, will host the PANCAP Knowledge for Health Treat All Strategy and Message Design Workshop from December 7-8 in Port-of-Spain, Republic of Trinidad and Tobago.
The Treat All policy, announced in September 2015 by the World Health Organisation (WHO), stated that anyone infected with HIV should begin antiretroviral treatment as soon after diagnosis as possible. With its “treat-all” recommendation, WHO removed all limitations on eligibility for antiretroviral therapy (ART) among people living with HIV; all populations and age groups are now eligible for treatment.
The workshop, designed to build the capacity of National AIDS Programme (NAP) Managers and representatives of Civil Society Organizations (CSOs) in creating strategic ‘Treat All’ messages, will host over 30 participants. It is an initiative of the PANCAP Knowledge for Health Project and will be facilitated by Beth Mallalieu, a Health Communications Specialist from the Johns Hopkins Centre of Communication Programmes and the PANCAP Knowledge for Health team.
Participants will be engaged in identifying target audiences (with a focus on key populations), selecting appropriate channels of communication and creating ‘Treat All’ messages that can be easily understood by key populations.
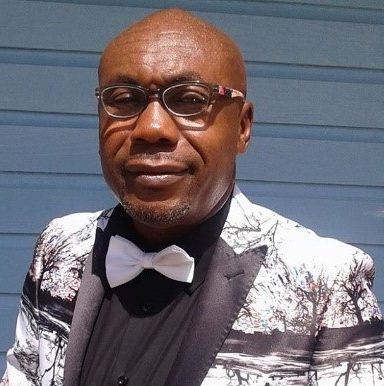
“We have listened to the needs of our civil society partners and NAP Managers and there is an urgent need for public education messages that explain the Treat All policy and benefits,’ stated Director of PANCAP, Dereck Springer, ‘we have developed a series of fact sheets on Treat All and the 90-90-90 targets; this workshop provides us with the opportunity to work directly with the Partnership to formulate strategic messages for key populations including Men who have sex with men, Sex workers and Youth within these key populations. It is essential that all stakeholders are educated about Treat All as we move to fast track the 90-90-90 targets”.
The workshop culminates a year of significant success for the Partnership with the relaunch of the Champions for Change initiative and specific interventions for CSOs, NAP managers, parliamentarians, youth, faith leaders and six countries in the region being certified as having achieved elimination of mother-to-child transmission of HIV and Syphilis.
Editor’s notes:
What is the ‘Treat All’ Policy?
Fact: Treat All policies could help avert more than 21 million deaths and 28 million new infections by 2030 (Source: World Health Organization).
In September 2015, the World Health Organization (WHO) issued a new policy, which stated that anyone infected with HIV should begin antiretroviral treatment as soon after diagnosis as possible. With its “treat-all” recommendation, WHO removed all limitations on eligibility for antiretroviral therapy (ART) among people living with HIV; all populations and age groups are now eligible for treatment.
The expanded use of antiretroviral treatment is supported by recent findings from clinical trials confirming that early use of ART keeps people living with HIV alive, healthier and reduces the risk of transmitting the virus to partners.
WHO now also recommends that people at “substantial” risk of HIV should be offered preventive antiretroviral treatment. This new recommendation builds on 2014 WHO guidance to offer a combination of antiretroviral drugs to prevent HIV acquisition, pre-exposure prophylaxis (PrEP), for men who have sex with men. Following further evidence of the effectiveness and acceptability of PrEP, WHO has now broadened this recommendation to support the offer of PrEP to other population groups at significant HIV risk. PrEP should be seen as an additional prevention choice based on a comprehensive package of services, including HIV testing, counselling and support, and access to condoms and safe injection equipment.
New recommendations on early use of ART and expanded offer of PrEP are contained in WHO’s “Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV.” The new guideline stresses that, in order to effectively implement the recommendations, countries will need to ensure that testing and treatment for HIV infection are readily available and that those undergoing treatment are supported to adhere to recommended regimens and are retained in care.
The recommendations were developed as part of a comprehensive update of the “WHO consolidated guidelines on the use of antiretroviral drugs for preventing and treating HIV infection”.
Based on the new recommendations, the number of people eligible for antiretroviral treatment increases from 28 million to all 37 million people who currently live with HIV globally. Expanding access to treatment is at the heart of the set of targets for 2020 with the aim to end the AIDS epidemic by 2030. These targets include 90% of people living with HIV being aware of their HIV infection, 90% of those receiving antiretroviral treatment, and 90% of people on ART having no detectable virus in their blood.
According to UNAIDS estimates, expanding ART to all people living with HIV and expanding prevention choices can help avert 21 million AIDS-related deaths and 28 million new infections by 2030.
CLICK HERE for the Guideline on when to start antiretroviral therapy and on pre-exposure prophylaxis for HIV.
What is PANCAP?
PANCAP is a Caribbean regional partnership of governments, regional civil society organisations, regional institutions and organisations, bilateral and multilateral agencies and contributing donor partners which was established on 14 February 2001. PANCAP provides a structured and unified approach to the Caribbean’s response to the HIV epidemic, coordinates the response through the Caribbean Regional Strategic Framework on HIV and AIDS to maximise efficient use of resources and increase impact, mobilises resources and build capacity of partners.
Contact:
Timothy Austin
Communications Specialist
PANCAP Coordinating Unit
CARICOM Secretariat
Turkeyen, Greater Georgetown, Guyana
Email: taustin.consultant@caricom.org
Tel: (592) 222-0001-75, Ext. 3409 | Visit www.PANCAP.org