Thursday, 7 October 2021 (PANCAP Coordinating Unit, CARICOM Secretariat): The Pan-Caribbean Partnership against HIV and AIDS (PANCAP), the mechanism that provides a structured and unified approach to the Caribbean’s response to the HIV epidemic, congratulates the eighteen (18) clinical and public health practitioners who completed the three-month course on the Clinical Management of HIV with the Global Health E-Learning Program (eDGH), University of Washington.
The PANCAP-USAID Project supported the capacity building initiative via USAID Jamaica.
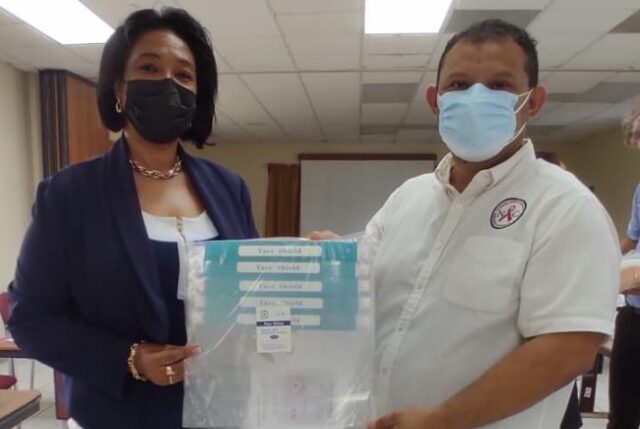
A certificate award ceremony was held on Friday, 1 October, at the Roraima Duke Lodge in Georgetown.
The CARICOM Secretariat, PANCAP and USAID were praised by Hon. Dr Frank Anthony, Minister of Health, Guyana, during his feature address. He underscored the importance of using the PANCAP initiative as an example of continuing programme implementation to end AIDS despite the disruptions caused by COVID-19.
Dr Anthony expressed gratitude to the U.S. Government and USAID for providing support for the initiative and highlighted the value of the course in improving the skills of the Public Health Practitioners and the overall enhancement the achievement will deliver to the Region’s public health.
The Minister of Health further praised the content of the course and stated that the inclusion of modules on Hepatitis B and C aligned with the Ministry of Health’s upcoming capacity building on the treatment of Hepatitis C.
Importantly, Dr Anthony highlighted that vaccination numbers for eligible People Living with HIV (PLHIV) were low. He attributed this to misinformation within the PLHIV community regarding the safety of the vaccines. He challenged the 18 certificate recipients to encourage PLHIV to get vaccinated by presenting facts on the safety and efficacy of the COVID-19 vaccines.
Dr Douglas Slater, Assistant Secretary-General, Human and Social Development, CARICOM Secretariat, delivered congratulations on behalf of Dr Carla Barnett, Secretary-General of the Caribbean Community (CARICOM). He echoed the sentiments of Dr Anthony and praised the initiative for prioritising knowledge sharing and learning among Public Health Practitioners despite the challenges of COVID-19.
“HIV and COVID-19 have taught us many lessons; pivotal to combating both is providing consistent opportunities for learning and capacity building for our front-line workers, doctors, nurses, and other public health workers”, stated Dr Slater, “PANCAP, with the support of the U.S. Government, USAID and through collaboration with the Ministry of Health, has taken a positive step towards this”.
“I was pleased that the course content contained modules critical for new thinking and innovative approaches for managing and treating HIV in the Region. These included topics focused on opportunistic infections, “Management of Sexually Transmitted Infections in HIV-infected Patients”, “HIV Vertical Transmission and Pregnancy”, “Post-exposure Prophylaxis for HIV and Preventive Care”, and “Pediatric HIV”, stated Dr Slater, “These areas are critical to creating a practical roadmap for ending AIDS in our Region”.
Dr Slater concluded by commending the PANCAP Knowledge Management hub for identifying and leveraging the Global Health E-Learning Program at the University of Washington. He also encouraged PANCAP to share the success story with the Region as many Public Health institutions continue to search for strategies and approaches for virtual learning. “Let this be a shining beacon of the progress the Region can achieve when we strategically collaborate and take full advantage of the fantastic opportunities of the virtual world”, stated Dr Slater.
Ambassador Sarah-Ann Lynch, United States Ambassador to the Co-operative Republic of Guyana, stated that the USAID Jamaica Office was proud to sponsor the initiative and praised the collaboration between USAID, CARICOM, and the Ministry of Health. She highlighted the importance of knowledge sharing and capacity building to the development of Guyana’s health sector. She emphasised that the U.S. Government was pleased to be part of the process.
The Ambassador stated that the commitment by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) to combat HIV is evidenced by the more than 185 Million United States Dollars provided in funding to Guyana since 2004. She also highlighted that the partnership has resulted in significant strides in HIV prevention, treatment and care in Guyana. The Ambassador was pleased to share that the PEPFAR programme received a two-year extension through the hard work of USAID and the Ministry of Health to help Guyana further its accomplishments in ending AIDS.
Ambassador Lynch concluded by congratulating the certificate recipients for having the vision of ending AIDS and stated that the U. S. Government remains committed to working with the Ministry of Health, CARICOM and the private sector to help this become a reality in Guyana.
Dr Rosmond Adams, Director, PANCAP, reiterated PANCAP’s commitment to building the capacity of Public Health Practitioners working in HIV prevention, treatment and care. He stated that the initiative would be the first of many partnering with international universities to enhance the capacities of clinical and public health workers.
Additional highlights included testimonials from three (3) doctors who completed the course, including Dr Tariq Jagnarine, Programme Manager, National AIDS Programme Secretariat (NAPS), Ministry of Health, Dr Mallika Mootoo, Paediatrician, Saint Joseph Mercy Hospital and Dr Abiola Jacobs, Director, National Care and Treatment Center. They reflected on the value of the course to their work implementation.
Certificate recipients included medical practitioners, programme managers, public health practitioners, medex and nurses from the Ministry of Health, Guyana, Society against Sexual Orientation Discrimination (SASOD), St. Joseph Mercy Hospital, Davis Memorial Hospital and CARICOM-PANCAP.
The capacity building initiative formed part of PANCAP’s overarching strategy to protect and maintain the gains made in the HIV response as the Region continues to navigate COVID-19.
– ENDS –
Contact:
Timothy Austin
Senior Project Officer, Communications
PANCAP Coordinating Unit
CARICOM Secretariat
Turkeyen, Greater Georgetown, Guyana
Email: taustin.consultant@caricom.org
Tel: (592) 222-0001-75, Ext. 3409 | Visit www.PANCAP.org
Helpful links:
Image Gallery:
https://photos.app.goo.gl/ZXpG7ypmbZbALUd59
Global AIDS Strategy 2021–2026, End Inequalities, End AIDS
https://pancap.org/pancap-documents/global-aids-strategy-2021-2026-end-inequalities-end-aids/
Caribbean Regional Strategic Framework on HIV and AIDS (CRSF) 2019-2025
https://pancap.org/pancap-documents/caribbean-regional-strategic-framework-2019-2025/
WHAT IS PANCAP?
PANCAP is a Caribbean regional partnership of governments, regional civil society organisations, regional institutions and organisations, bilateral and multilateral agencies and contributing donor partners which was established on 14 February 2001. PANCAP provides a structured and unified approach to the Caribbean’s response to the HIV epidemic, coordinates the response through the Caribbean Regional Strategic Framework on HIV and AIDS to maximise efficient use of resources and increase impact, mobilises resources and build capacity of partners.
EDITOR’S NOTES
What are the Global AIDS Strategy 2021–2026 targets and commitments?
If targets and commitments in the strategy are achieved:
- The number of people who newly acquire HIV will decrease from 1.7 million in 2019 to less than 370 000 by 2025
- The number of people dying from AIDS-related illnesses will decrease from 690 000 in 2019 to less than 250 000 in 2025.
- The goal of eliminating new HIV infections among children will see the number of new HIV infections drop from 150 000 in 2019 to less than 22 000 in 2025.
Image Gallery – Clinical Management of HIV – Certificate Award Ceremony