In a landmark speech to a United Nations High-Level Meeting on HIV and AIDS on Tuesday, President Irfaan Ali declared that Guyana would make HIV-related discrimination illegal and address the needs of key populations.
Guyana looks to end AIDS as a public health threat in the next ten years.
President Ali said that Guyana would make discrimination against people with HIV “unacceptable, illegal, and punitive, throughout society, including Government, the private sector and civil society.”
He said that in the coming years, Guyana would strive to reach “vulnerable groups such as LGBTI (Lesbians, Gays, Bisexual, Transgender, Intersex), sex workers and immigrants.”
The President said Guyana would focus on integrating mental health in all HIV policies and programmes and transforming the current paper-based HIV monitoring system into an IT-based system.
“The Government of Guyana is fully committed to providing universal access to prevention, care and treatment for everyone living with HIV or living under the threat of HIV infections,” the President stated.
He noted that Guyana’s HIV programme results are among the best in the Caribbean. A total of 95% of those living with HIV have been diagnosed. Seventy-three (73%) percent who are aware of their HIV status are on treatment and, almost nine out of every ten of these were virally suppressed.
He also noted that over the past 20 years, Guyana had reduced new HIV infections by more than half in Guyana. While impressive, like many countries around the world, we came close but missed the UN 2020 90-90-90 Targets. In the 2021-2025 period, Guyana is committed to reaching the new UNAIDS global 95-95-95 goal.
According to the President, Guyana has already embarked on a comprehensive Pre-Exposure Prophylaxis programme, ensuring that anyone, anywhere in Guyana, who is at risk of an HIV infection, can access Pre-Exposure Prophylaxis.
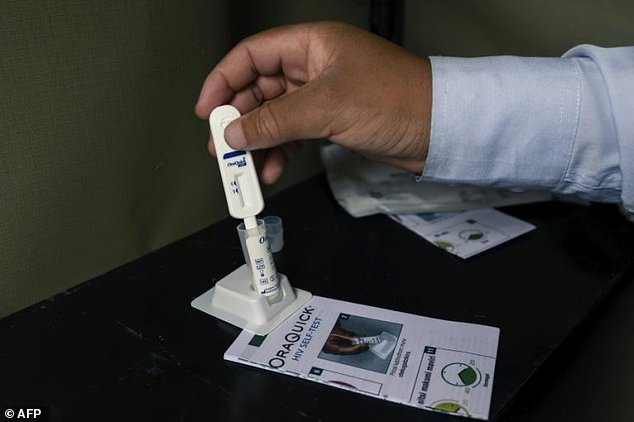
“Another innovative focus of our comprehensive response is increasing self-testing,” the President stated.
“We have already integrated testing, diagnosis and treatment for sexually transmitted diseases in our primary health care system. In addition, we are committed to the elimination of gonorrhoea and syphilis in our maternal population.”
See the President’s full speech below:
Secretary-General;
Distinguish Heads of State;
Other Distinguish Delegates;
When my country launched its HIV National Strategic Plan 2021-2025, we re-committed to the UNAIDS Global AIDS Strategy, which aspires to end AIDS as a public health threat by 2030.
The Government of Guyana is fully committed to providing universal access to prevention, care and treatment for everyone living with HIV or living under the threat of HIV infections.
Guyana’s HIV programme results are among the best in the Caribbean. A total of 95% of those living with HIV have been diagnosed. Seventy-three (73%) percent who are aware of their HIV status are on treatment and, almost nine out of every ten of these were virally suppressed.
Over the past 20 years, Guyana has reduced new HIV infections by more than half in Guyana. While impressive, like many countries around the world, we came close but missed the UN 2020 90-90-90 targets. In the 2021-2025 period, Guyana is committed to reaching the new UNAIDS global 95-95-95 goal.
Guyana has already embarked on a comprehensive Pre-Exposure Prophylaxis programme, ensuring that anyone, anywhere in Guyana, who is at risk of an HIV infection, can access Pre-Exposure Prophylaxis.
Another innovative focus of our comprehensive response is increasing self-testing. We have already integrated testing, diagnosis and treatment for sexually transmitted diseases in our primary health care system. In addition, we are committed to the elimination of gonorrhoea and syphilis in our maternal population.
Other key areas of focus in Guyana for the coming period include:
Making the discrimination of HIV unacceptable, illegal, and punitive, throughout society, including Government, the private sector and civil society;
Reaching vulnerable groups such as LGBTI, sex workers and immigrants;
Integrating mental health in all HIV policies and programmes and transforming the current paper-based HIV monitoring system into an IT-based system.
Guyana is keen on ensuring that these areas of focus are reflected in the 2021 Political Declaration.
Distinguished Delegates,
As we gather again for another High-Level Conference on HIV, as we observe the 25th anniversary of the formation of UNAIDS, the global inequity that facilitated AIDS to leave a trail of death for forty years is very much evident as we combat the COVID-19 pandemic. The truth is we still live in two very different worlds. COVID-19 vaccine inequity is a moral dilemma.
Our 2021 Political Declaration emanating out of this meeting must ensure funding for UNAIDS and the Global Fund.
This 2021 High-Level meeting must become a trigger for concerted and sustained action over the next decade to root out the conditions that contribute to and fuel the HIV pandemic.
I thank you.